


Received: 07-Feb-2022, Manuscript No. GJDOH-22-58886; Editor assigned: 10-Feb-2022, Pre QC No. GJDOH-22-58886 (PQ); Reviewed: 24-Feb-2022, QC No. GJDOH-22-58886; Revised: 02-Mar-2022, Manuscript No. GJDOH-22-58886 (R); Published: 09-Mar-2022, DOI: 10.15651/2449-1918.22.9.001
Oral health refers to the health of the teeth, gums, and the entire oral-facial system that allows us to smile, speak, and chew.
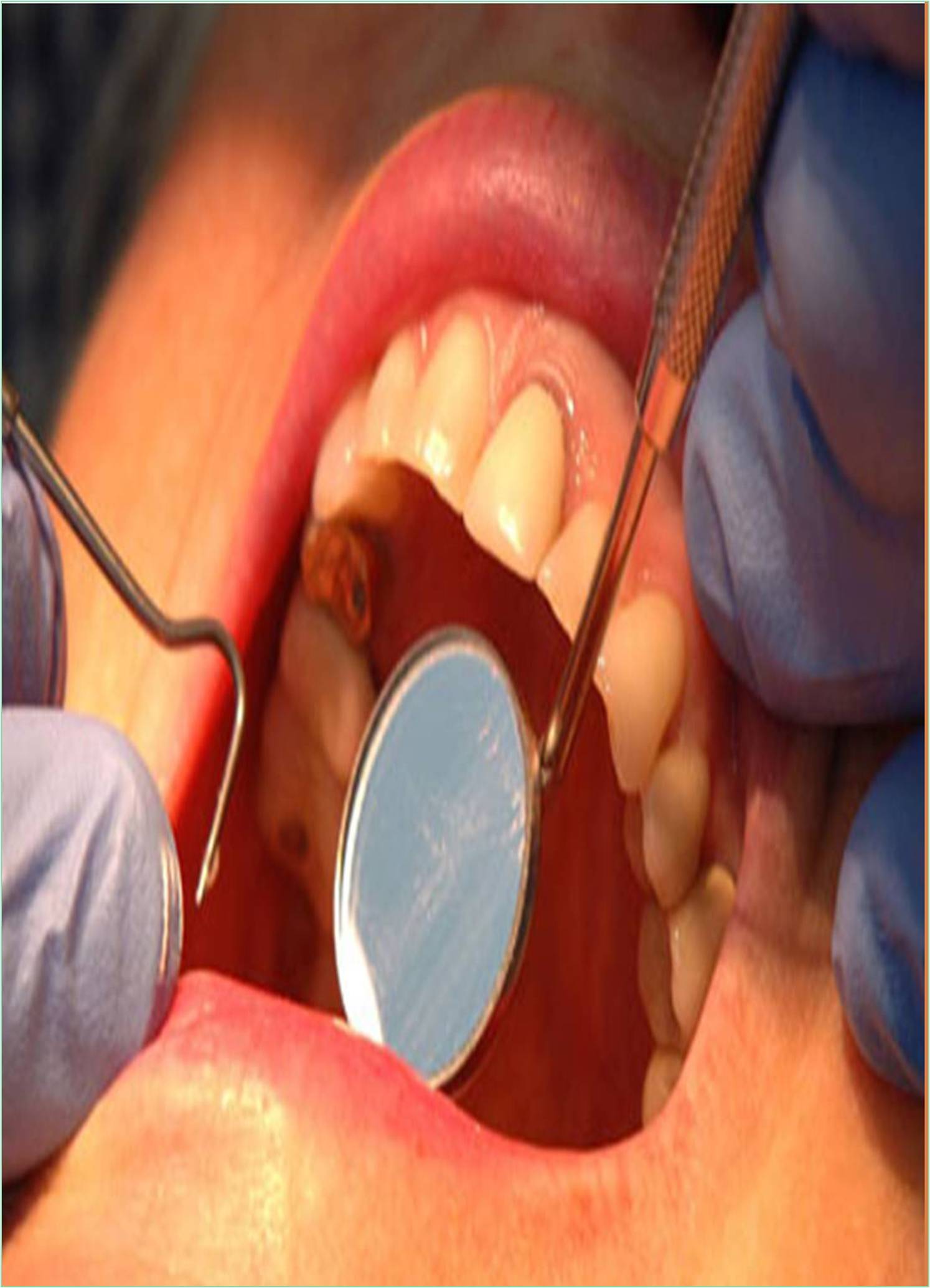
Periodontitis, or gum disease, is a common infection that damages the soft tissue and bone supporting the tooth. Without treatment, the alveolar bone around the teeth is slowly and progressively lost.
Periodontitis is common but largely preventable. It’s usually the result of poor oral hygiene. Brushing at least twice a day, flossing daily and getting regular dental checkups can greatly improve chances of successful treatment for periodontitis and can also reduce chance of developing it.
Untreated periodontitis ultimately leads to tooth loss. It may increase the risk of stroke, heart attack and other health problems.
Plaque, a sticky, colourless film that forms on the surface of teeth, is the most common cause of periodontitis. If plaque is not removed, it can harden and form tartar or calculus.
Symptoms
• Gums that bleed, grow red, swollen, tender and also recede (tissue pulls back, so more of the teeth show).
• Teeth that become loose, feel sensitive, get surrounded by pus and look like they’re longer (from receding gums).
• Other symptoms include- bad breath, change in bite (way lower and upper teeth come together) and also painful chewing.
Causes
In most cases, the onset of periodontitis begins with plaque. Plaque is a sticky film made primarily of bacteria. If left untreated, plaque can eventually lead to periodontitis.
• When starch and sugar in food interact with bacteria that are normally in the mouth, plaque forms on the teeth. Brushing teeth twice a day and using dental floss once a day will remove the plaque, but it re-forms quickly.
• If plaque remains on your teeth, it can get harden under gums and become tartar. Tartar is difficult to remove and is filled with bacteria. The longer the plaque and tartar that remains on the teeth, the more damage it can do. Tartar cannot be removed by brushing or dental floss. Professional cleaning is required to remove tartar.
• Dental plaque can cause gingival inflammation, the mildest form of gum disease. Gingivitis is irritation and inflammation of the part of the gingival tissue (gingiva) around the root of the tooth. Gingivitis can be remedied with professional treatment and proper oral care at home.
• Persistent gingival inflammation can cause periodontal disease, eventually forming a plaque, tartar, and bacterial-filled pocket between the gums and teeth. Over time, these pockets get deeper and fill with more bacteria. If left untreated, these deep infections cause tissue and bone loss, which can eventually lead to the loss of one or more teeth. Persistent chronic inflammation can also strain the immune system.
Risk Factors for Periodontitis
Periodontal disease is fairly rare in people under the age of 30. Still, it can affect people with poor oral hygiene, who do not brush their teeth or floss regularly.
However, periodontitis is more likely to occur with age. Years of poor oral hygiene have been their victims. Before have periodontitis, gingival inflammation is developed, which is a less severe. Periodontitis can occur if you are not treated for gingival inflammation.
Men are also more likely to develop periodontitis. One possible reason is that men are less likely to receive regular dental treatment.
Other factors that can increase your periodontitis risk include
• Smoking (most significant factor), since it weakens the body’s ability to fight infection.
• Diabetes, since people with diabetes are at higher risk for developing infections.
• Medications that lower the production of saliva, which protects your gums. These medicines include antihistamines, antidepressants and drugs for hypertension (high blood pressure).
• Genetics — you may have genes that put you at higher risk.
• Hormonal changes in women, such as pregnancy or using birth control pills.
• Diseases that limit the immune system’s response, such as cancer or AIDS. These conditions can lead to necrotizing periodontitis, the most severe form.