


Received: 30-Nov-2022, Manuscript No. GJDOH-22-82936; Editor assigned: 02-Dec-2022, Pre QC No. GJDOH-22-82936 (PQ); Reviewed: 16-Dec-2022, QC No. GJDOH-22-82936; Revised: 23-Dec-2022, Manuscript No. GJDOH-22-82936 (R); Published: 30-Dec-2022, DOI: 10.15651/2449-1918.22.9.011
General health and wellbeing are inextricably linked to oral health. Global economics and public health are severely impacted by oral disorders, which also dramatically lower the quality of life for individuals who are affected. According to the Global Burden of Disease survey, oral diseases impacted 3.9 billion people. The most common oral disorders worldwide are periodontal disease and dental caries (tooth decay). Moreover half of the world's population had periodontal disorders, with severe periodontitis affecting 11.2% of the population. Similar to how dental caries, which affects over 2.4 billion people, is most common in permanent teeth, early childhood caries, which affects 621 million children, is a hidden worldwide epidemic that has a detrimental impact on children's quality of life and well-being. The cumulative burden of oral illnesses and ailments has greatly grown as a result of changes in demographic profiles, especially the ageing population. Untreated oral disorders affected 3.5 billion persons worldwide in 2015, up from 2.5 billion in 1990, with a 64% rise in Disability Adjusted Life Years (DALYs).
Globally, oral illnesses and disorders continue to be a public health burden, with particular issues in many nations linked to wealth disparity and economic developments. Even though many oral illnesses are mostly avoidable, their continued high prevalence is a sign of inequality and a lack of funding, particularly in underprivileged areas or low- and middle-income nations. Oral illnesses and ailments follow a societal pattern, much as the bulk of these diseases. The majority of children with dental caries and those from socially excluded groups have limited access to dental treatment. Because of inadequate financial and personnel resources, the great majority of oral illnesses in underdeveloped nations go untreated. These expenses place financial strain on the health care industry as well as on families. A broader social framework that takes behavioural, biological, psychological, economic and political influences into account is currently recommended as a more effective way to investigate the causes of chronic illnesses, including oral disorders, and the distribution of health disparities. There are still significant disparities in oral health both within and across nations.
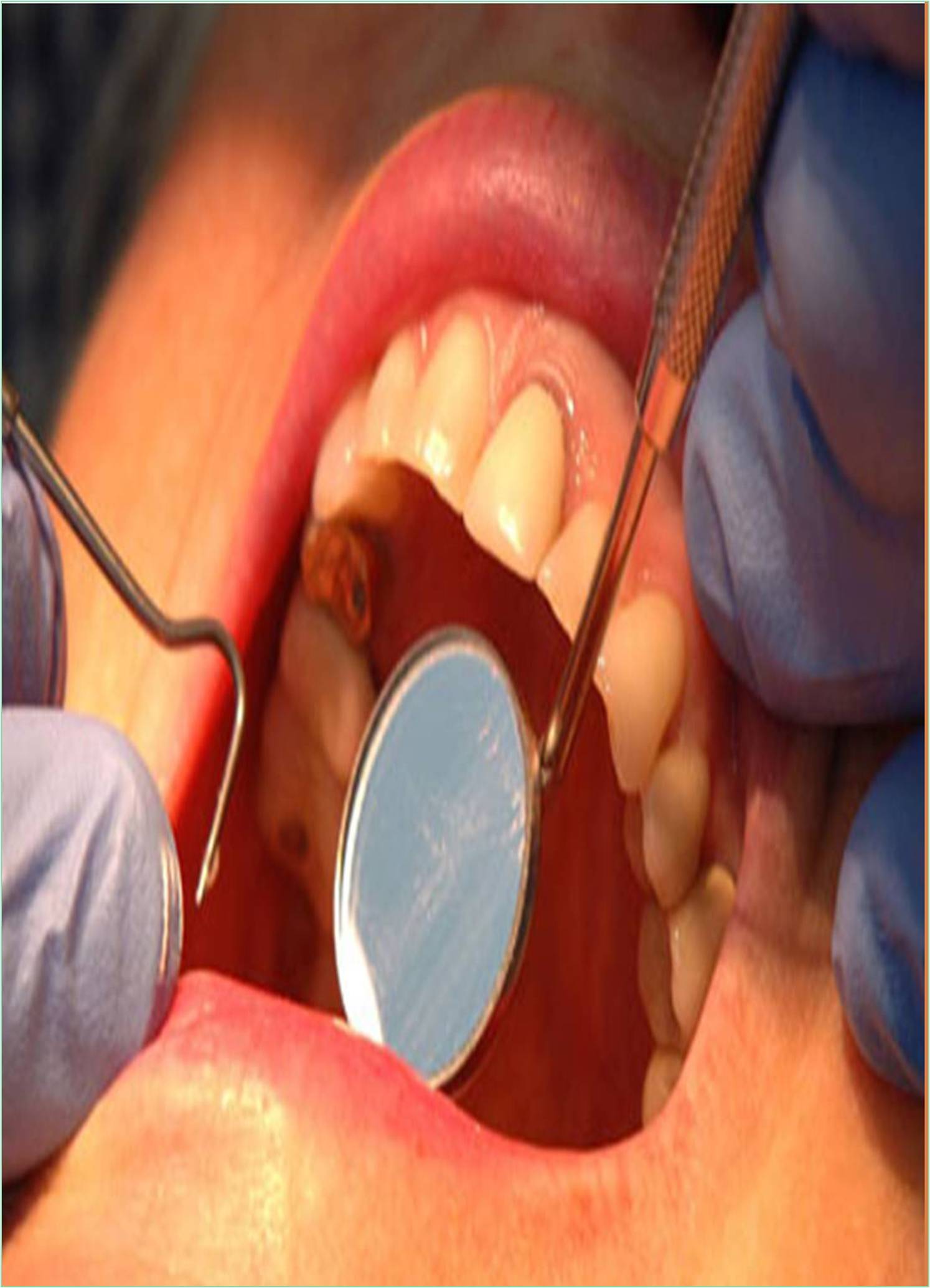
Patients with dry mouth have a significant failure rate for restorations. These trials, however, lacked a comparison group of patients with normal salivary flow rates, thus it is not known how much dry mouth affects restoration survival. The longevity of restorations is influenced by a number of factors, including the patient's age, sex, and dental hygiene as well as the patient's tooth type, restoration material, and size. The repair material is particularly interesting among these qualities since, if chosen well, it may make up for the other undesirable ones. Research on restoration survival in patients with dry mouth have only looked at direct restorations, therefore there aren't any direct vs. indirect material comparisons in those studies. The longevity of various restoration materials in dry mouth patients must be evaluated in order to offer them with individualised dental treatment. The objectives of this practice-based retrospective data collecting study were thus to I quantify the impact of dry mouth on restoration and tooth survival, and ii) compare the longevity of various restoration materials in dry mouth patients.
When compared to restorations in control patients, the dry mouth patients' restorations had a 2.08-fold hazard ratio (95% CI: 1.65-2.63), according to the first multivariate Cox regression analysis. The study was modified to account for the patient's sex, age, tooth type, restoration size, and material. The results of the second multivariate Cox regression analysis showed that individuals with Sjögren's disease or a history of radiation to the head or neck had a considerably greater hazard ratio for restorations. The risk ratios according to tooth type and patient gender were lower than those related to restoration material and size. In order to ascertain the impact of leaving out the patient variables of sex and age, the third multivariate Cox regression analysis was conducted to examine the hazard ratios for dry mouth, restoration material, number of surfaces, and tooth type. The individuals with dry mouth had significantly shorter restoration and tooth survival times. Their fixed prosthetic crowns had a respectable survival rate, but particularly their massive composite fillings (covering four or five surfaces) and glass ionomer cement fillings had low survival times. It is important to remember that dry mouth patients' restorations and teeth have a much shorter life period when discussing the predicted survival of a restoration with them.