


Received: 07-Feb-2022, Manuscript No. GJDOH-22-59748; Editor assigned: 10-Feb-2022, Pre QC No. GJDOH-22-59748 (PQ); Reviewed: 24-Feb-2022, QC No. GJDOH-22-59748; Revised: 02-Mar-2022, Manuscript No. GJDOH-22-59748 (R); Published: 09-Mar-2022, DOI: 10.15651/2449-1918.22.9.005
Mandibulectomy is a surgical operation in which the mandible (jaw), a crucial bone in the face that contributes substantially to mastication or chewing, is removed or resected. There are many types of mandibulectomy relying on the thickness and extent of resection required. In hemimandibulectomy, half of the mandible is removed.
As patients are not allowed to eat by mouth immediately after, the procedure is typically followed by the insertion of a tube from the nose into the stomach to allow feeding during the recovery period. Patients are also scheduled for follow-ups, which typically involves physical examinations and imaging studies, such as a CT scan, to ensure the success of the procedure.
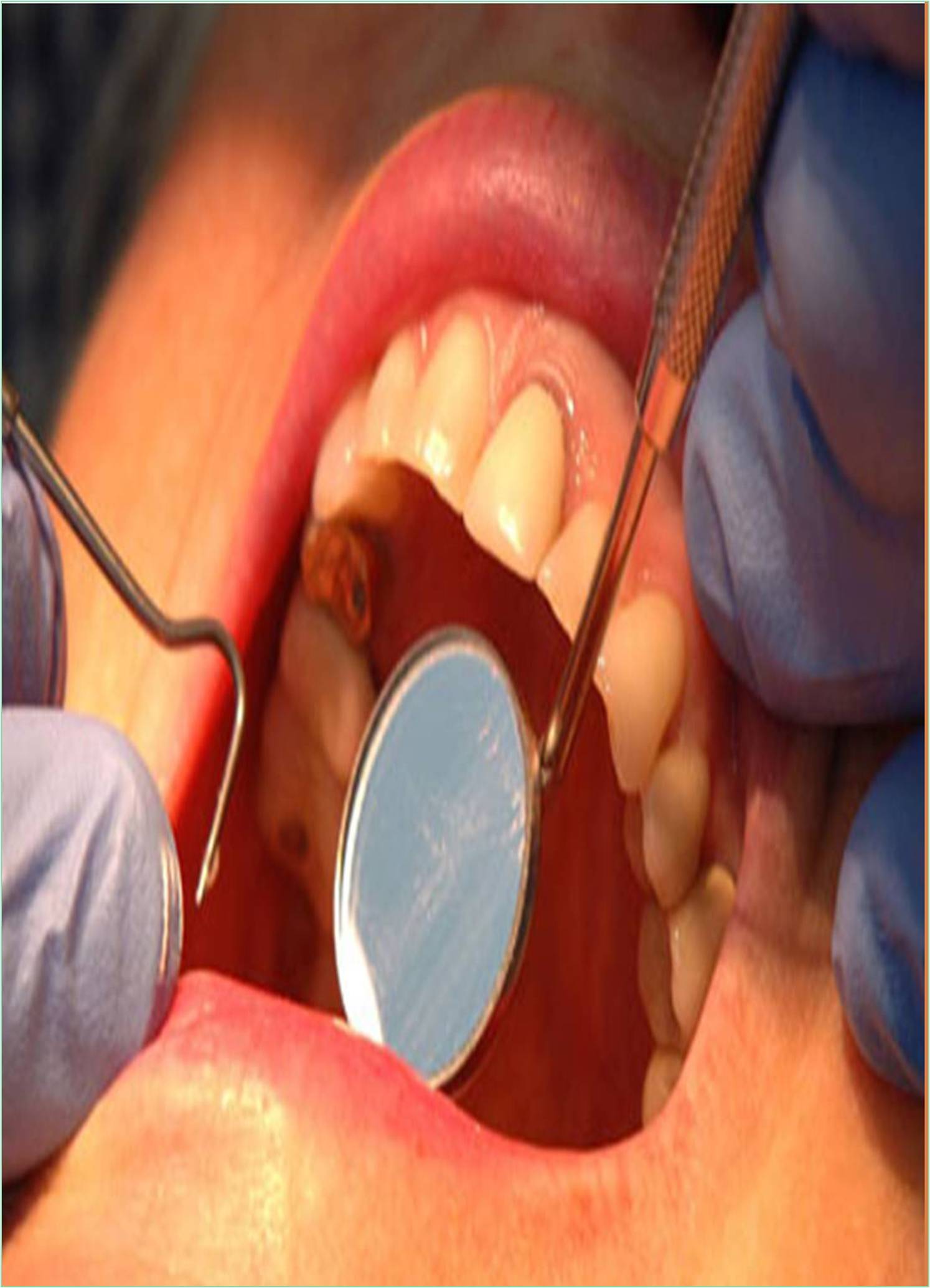
Hemimandibulectomy is the major surgery performed under general anesthesia. It is typical approach with combined incisions in the face and neck, transcervically. In some cases, splitting of lip is necessary for proper exposure and easy access to the mass. Ameloblastoma is a benign neoplasm, odontogenic in nature and associated with high recurrence rate (Varkhede et al., 2010). Treatment modality thereby warrants a wide excision to reduce the possibility of recurrence (Olaitan et al., 1998). Post-surgical re - habilitation is a challenging task for the prosthodontist as resection results in deviation and downward rotation of the mandible that alters the maxillomandibular relationship impairing the function, speech, and aesthetics to a great extent (Curtis et al., 1974). Guide Fange Prosthesis (GFP) is a mandibular conventional prosthesis useful to the patient who is not consistently able to achieve appropriate mediolateral position of the mandible required for adequate mastication (Desjardins, 1979).
The GFP prosthesis prevents the mandible from deviation while speaking and in function. Loss of mandibular continuity results in deviation of remaining mandibular segment toward the resected side primarily because of the loss of tissue involved in the surgical resection. The final outcome of prosthetic rehabilitation is based on various factors, the most important of all is the extent of the surgical resection, the presence of mandibular continuity and patient’s cooperation and psychological wellbeing (Majage et al., 2010). The earlier the mandibular guidance therapy is initiated in the course of treatment; the more successful is the patient’s definitive occlusal relationship. This case report describes prosthodontic management of a patient who has undergone a hemimandibulectomy and was rehabilitated using provisional guide flange prosthesis followed by definitive fixed cantilever prosthesis.
The recent advances in the field of maxillofacial prosthodontics have changed the outlook in rehabilitation of hemimandibulectomy patients. With the advent of newer materials, promising results can be achieved in challenging cases (Marathe et al., 2016). There are many treatment options for restoring the defect like guiding flange prosthesis, conventional acrylic removable partial prosthesis, cast partial dental prosthesis, implants etc. The choice of treatment depends upon the size of resection, the amount of deviation, patient’s overall wellbeing, socioeconomic status and patient’s cooperation (Kar et al., 2015). According to a study the edentulous patients who have experienced mandibular resection with no recurrence for a year are candidates for prosthetic treatment. However, most of the cases deal with partially edentulous patients and very few are related to completely edentulous patients.
Curtis TA, Cantor R (1974). The forgotten patient in maxillofacial prosthetics. J Prosthet Dent. 31(6): 662-680. [Crossref] [Google Scholar]
Desjardins RP (1979). Relating examination findings to treatment procedures. In: Laney WR, editor. Maxillofacial prosthetics. 69-114. [Google Scholar]
Kar S, Tripathi A, Madhok R (2015). Treatment outcome with guiding flange prosthesis in hemimandibulectomy patients: Case series of three patients. Ann Maxillofac Surg. 5(2): 266-270. [Crossref] [Google Scholar]
Majage B, Chandrakar N, Chowdhary R, Gala V, Moldi A, Mahoorkar S (2010). Prosthodontic rehabilitation of hemi mandibulectomy patient with magnet retained overdenture - A case report. Int J Clin Dent Sci. 1: 30-32. [Crossref] [Google Scholar]
Marathe AS, Kshirsagar PS (2016). A systematic approach in rehabilitation of hemimandibulectomy: A case report. J Indian Prosthodont Soc. 16(2): 208-212. [Crossref] [Google Scholar]
Olaitan AA, Arole G, Adekeye EO (1998). Recurrent ameloblastoma of the jaws: A follow-up study. Int J Oral Maxillofac Surg. 27: 456-460. [Crossref] [Google Scholar]
Varkhede A, Tupkari JV, Mandale MS, Sarda M (2010). Plexiform ameloblastoma of mandible: Case report. J Clin Exp Dent. 2: 146-148. [Crossref] [Google Scholar]